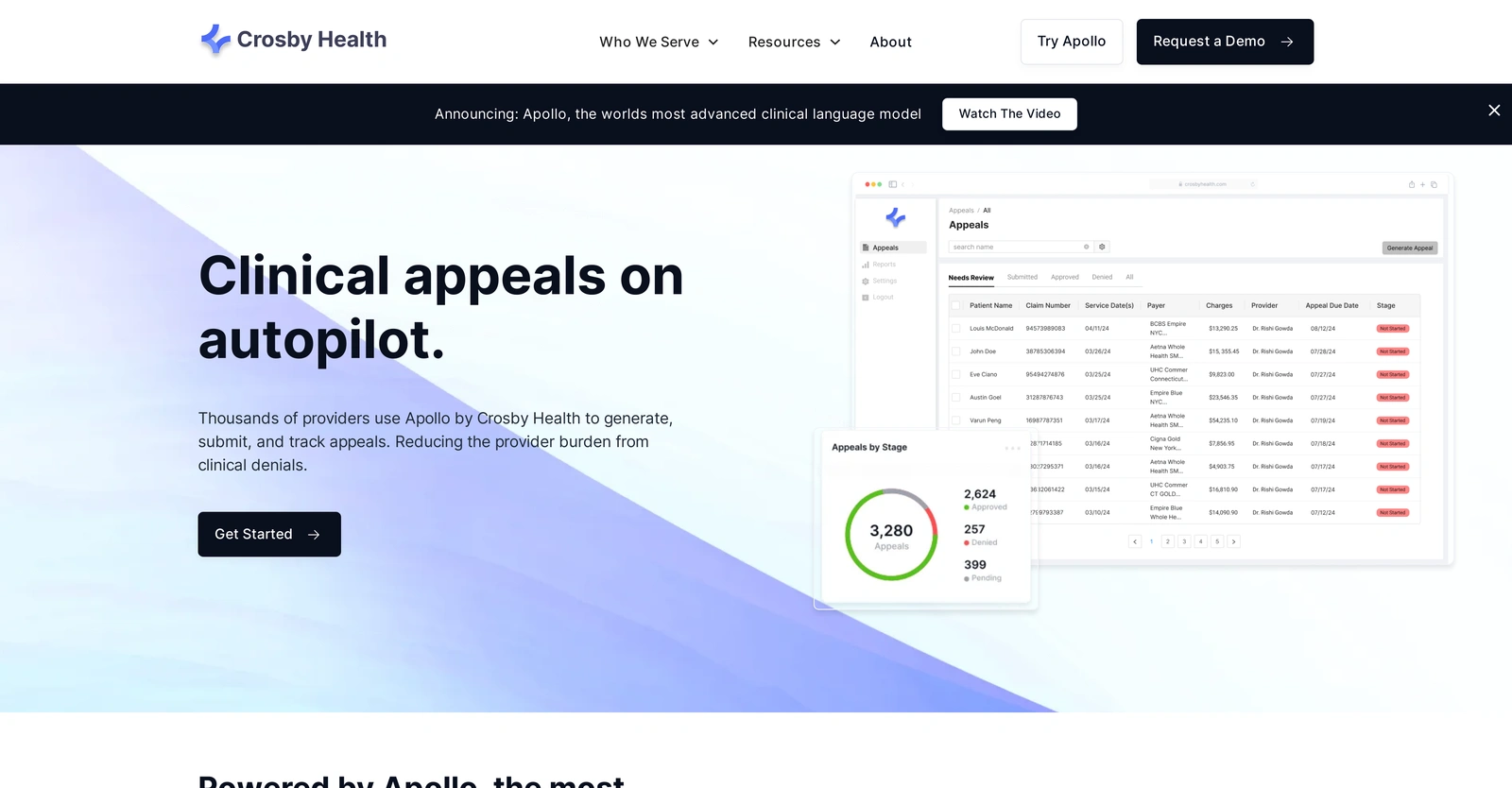
Apollo by Crosby Health is an advanced clinical appeal tool utilized by various healthcare providers. These include hospitals, health systems, private practices, and revenue cycle management providers. It automates clinical appeals processes, reducing the burden from clinical denials. Apollo has been trained on a vast repository of clinical encounters to handle clinical language and understand related tasks. Apart from medical knowledge, Apollo is designed to comprehend billing tasks, such as auditing, charge capture, and denial management. Its proficiency lies in crafting meticulous arguments for appeal letters for every denial with the goal of maximum recovery. The tool also eliminates the provider’s burden of generating appeals. It is trained to identify medical necessity within documentation, integrates legal and clinical guidelines, and facilitates unified submission to every payor. The platform is designed to automate tracking and confirmation of receipt, and it provides immediate notifications of payor decisions. The focus is to create a centralized platform that generates, submits, and tracks denial appeals, thereby eliminating the necessity of multiple payor portals. Critically, the tool offers one-click submission to any insurance company.
Description
Get to know the latest in AI
Join 2300+ other AI enthusiasts, developers and founders.
Thank you!
You have successfully joined our subscriber list.
Add Review
Pros
Automates clinical appeals processes
Automates tracking and confirmation
Centralized platform for denial appeals
Charge capture capability
Creates meticulous appeal letters
Eliminates burden of generating appeals
Eliminates need for multiple payor portals
Fast clinical language model
Fine-tuned understanding of billing tasks
Handles clinical language
High precision auditing
Identifies medical necessity in documentation
Immediate notifications of payor decisions
Integrated appeal management
Integrates legal and clinical guidelines
Large context length capacity
Maximum recovery goal
One-click submission to insurance
Reduces provider burden from denials
Revenue cycle management function
Suitable for various healthcare providers
Trained on vast clinical encounters
Understands billing tasks
Unified submission to every payor
Automates tracking and confirmation
Centralized platform for denial appeals
Charge capture capability
Creates meticulous appeal letters
Eliminates burden of generating appeals
Eliminates need for multiple payor portals
Fast clinical language model
Fine-tuned understanding of billing tasks
Handles clinical language
High precision auditing
Identifies medical necessity in documentation
Immediate notifications of payor decisions
Integrated appeal management
Integrates legal and clinical guidelines
Large context length capacity
Maximum recovery goal
One-click submission to insurance
Reduces provider burden from denials
Revenue cycle management function
Suitable for various healthcare providers
Trained on vast clinical encounters
Understands billing tasks
Unified submission to every payor
Cons
Absence of an API
Closed-source system
Lack of flexibility in customization
Limited to the healthcare industry
No integration with EHR systems
No multilingual support
No offline functionality
No role-based access control
No user access control
Single insurance company submission
Closed-source system
Lack of flexibility in customization
Limited to the healthcare industry
No integration with EHR systems
No multilingual support
No offline functionality
No role-based access control
No user access control
Single insurance company submission
Alternatives
Promote Your AI Tool
Get seen by thousands of AI enthusiasts, founders & developers.
- Homepage, Search and Sidebar Ads
- Featured Placements
- Click Stats & more
AI News








Leave a Reply